Ophthalmology Specialists On The Future Of Cataract Surgery
personalEYES | 7 Sep 2019

Following our recent interview with Dr Jose Luis Guell, we talked to another two major figures that appeared on this year’s RANZCO congress. We are honored to present the views of the renowned Australian ophthalmologists, Noel Alpins, MD, FACS and Clinical Assoc. Prof. Michael Lawless, who were kind enough to share their opinions on future trends in cataract surgery.
RANZCO congress impressions
As noted by both of our correspondents, this year’s RANZCO congress was a notable event for international eye specialists, who had a unique chance to exchange their experiences and hear some excellent presentations. In relation to the congress, Professor Alpins notes:
”The 2014 RANZCO scientific congress held in Brisbane this November was an outstanding academic event thanks both to the five international speakers whose contributions were substantial, together with presentation from fellows from all over Australia and New Zealand.”
Similarly, Dr Michael Lawless shares his positive impressions about the congress program and organization: ”The two principal guests for the RANZCO conference in Brisbane in late 2014 were Professor Jose Guell from Barcelona, Spain, and Professor Terence O’Brien from Miami, Florida. Both are world experts in corneal, cataract, refractive and external ocular disease. RANZCO was fortunate to have two people who are not only entertaining speakers, but also have a wealth of clinical knowledge and research experience not often seen together.”
Cataract Surgery Trends: Dr Alpins
Speaking about the congress, Professor Alpins notes that Cataract Surgery sessions were popular and well attended with a few topics that were highly relevant and in various stages of their evolutionary development. He specifically mentions Femto cataract surgery that seems to have had ”much exposure but the two points of interest were the association of endothelial loss and the Femto-laser incisions, compared to manual blade incisions. The winning poster demonstrated no statistical significant difference in visual outcomes between laser and conventional phaco and that cost effectiveness of laser not yet demonstrated.”
As for the topics that are likely to become more influential in improving Cataract outcomes in 2015, Dr Alpins gives an elaborate answer:
”Toric implants featured prominently with the means to determine more accurately the astigmatism magnitude and meridian by the CorT parameter (corneal topography astigmatism) from topographers and tomographers for total power CorT. Toric calculations are now possible on line with a free generic toric calculator (www.assort.com) that includes features such as, device refractive index, axial length, optimised lens constant for ELP and vertex toric power to corneal plane. This calculator has the unique feature of all implants on its selection set and there is also a clinically useful refractive surprise calculator for when excess refractive cylinder remains. Intraoperative alignment with either the Veryon or Callisto was also demonstrated to be beneficial over manual marking techniques. The place of intraoperative aberrometry is yet to be confirmed.
Finally at the end of the cataract procedure, intraoperative antibiotics such as Cephazolin are associated with reduced incidence of endophthalmitis. A show of hands confirmed that the vast majority of cataract surgeons now employ the prophylactic treatment which is on its way to becoming standard of care.”
5 Topics of Discussion: Dr Lawless
Since Dr Lawless was, as he himself points out, lucky to have hosted a session specifically on the topic of what Dr Guell and Dr O’Brien had done differently in the past year, he gives a detailed overview of the most interesting themes discussed during the session.
1. Paying attention to the ocular surface prior to surgery;
The first thing they both agreed on was what is perhaps very simple, but necessary to get the best from cataract and intraocular lens surgery. That is, paying attention to the ocular surface prior to surgery. This means conducting diagnostic tests to discover mild dry eye disease or lid margin inflammation that can contribute to an unstable tear film. There are several reasons that this is important to sort out ahead of time, not only because ocular surface disease can compromise the measurements necessary for selecting the correct intraocular lens. Consideration of the ocular surface can also help guide what type of intraocular lens to use, whether it be multifocal or monofocal. In addition, pre-treating ocular surface disease allows for a quicker, more comfortable visual recovery post-operatively.
There are some new diagnostic tests that assess tear osmolality, which they are using routinely, and also new techniques to treat the meibomian glands. The oil produced in the meibomian glands is essential to tear film stability and important in controlling ocular surface inflammation. Blockage or abnormalities in these glands can be treated these days with intense pulsed light or heat and mechanical massage to express the oil. There are various devices which are starting to become available to treat meibomian gland inflammation and blockages in a way that not only symptomatically helps the patients in routine practice, but also particularly improves their ocular surface health prior to cataract surgery. This is not commonly done in Australia, but I think will be brought into clinical practices over the next few years. It means taking a step back and considering some things which cataract surgeons don’t always put the front of their mind at the time of surgical decision-making.
2. Choosing the appropriate intraocular lens for the patient;
There is no consensus on the best intraocular lens, although both surgeons agreed that the qualities of biocompatibility, lens stability within the capsular bag and rotational stability, particularly when dealing with toric lenses, were the most important features in deciding which lens to use. The jury was out on whether to use the newer-style trifocal lenses or the more commonly used defractive multifocals, or whether to use aspheric lenses which induce some spherical aberration to improve depth of focus, but they all have their good and bad points. There was no one magic lens, but the message was that in the next year, just as in the past year, the lens choice will need to be a decision based not only on the patient’s corneal anatomy and ocular health, but also a communication between surgeon and patient as to what type of lens would suit their personality and lifestyle best. This is a conversation which requires some time, and, in order for the patient to gain the most from cataract surgery, a conversation which it is necessary to have. As always, there are some new lens designs in the pipeline. Perhaps the most interesting is the light-adjustable lens, which, once placed in the eye, can be treated to refine refractive errors. Professor Guell in particular, felt the time was coming when this lens design would be more commonly available, although he readily admitted that it has been a long time getting to this stage.
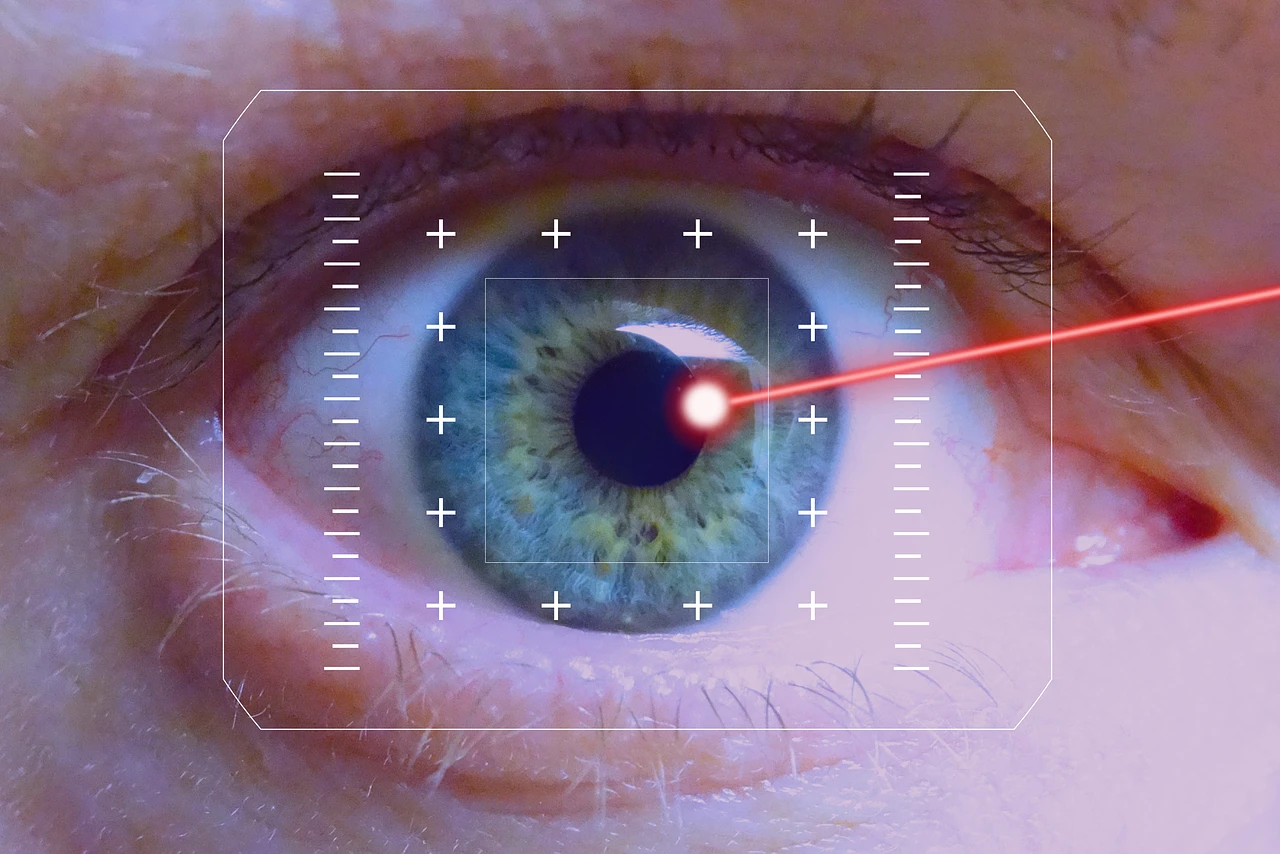
3. Using a femtosecond laser;
Using a femtosecond laser to assist in parts of the cataract procedure was routinely performed by both Professors Guell and O’Brien. They felt that it added some modest safety and accuracy benefits for their patients and had particular application in certain conditions where the eye was at higher risk of complications, such as Fuchs’ corneal dystrophy or pseudoexfoliation. They agreed that femtosecond laser is certainly not essential and routine phacoemulsification, particularly with the newer Centurion device, is still a very safe procedure.But in practice they would both be having laser cataract surgery themselves when the time came. They also understood that the data to justify this was still coming through in the literature and there are some controversies regarding the laser’s effect on the anterior capsule, which are still to be reconciled.
4. Using technology for surgical guidance;
Both Professors Guell and O’Brien used digital technology for surgical guidance. By this I mean instruments which digitally analysed the pupil and ocular landmarks so that the surgeon can place the intraocular lens in exactly the position that they wish. This goes for all intraocular lenses, but particularly in astigmatic-correcting toric intraocular lenses where the alignment is critical for a good result. The manual methods used in the past have effectively been surpassed by digital methods and the various companies responsible for these devices are attempting to integrate these so that the machines talk to each other in the operating room and in the laser suite. Both Professors have embraced these technologies and with good reason. Any improvement by automation or digitisation over manual methods intuitively makes sense, and this is certainly their opinion, particularly regarding toric intraocular lens placement.
5. Performing thinner posterior corneal transplants;
On the corneal transplant side, both surgeons were of the opinion that deep stromal endokeratoplasty is moving to Descemet’s membrane endokeratoplasty; that is, even thinner and thinner posterior corneal transplants. These are not without their problems; the steep learning curve for surgeons as well as the inadequate supply of tissue can be impediments to using these techniques satisfactorily. Despite this, both Professors felt that this was the direction in which corneal transplantation was heading.
Conclusions
As our correspondents note, 2014 was truly an interesting year in cataract surgery and 2015 is expected to be even more so, especially considering the latest trends. Professor Lawless points out that ”these are some good things for ophthalmologists in Australia to consider, some of which are currently being used and some which would be new to many Australian surgeons. The profession continues to creep forward in a way that is always a little confronting in terms of how to implement new techniques and technologies, how to pay for them and how to introduce them into clinical practice. ”
About Professor Lawless
Clinical Assoc. Prof. Michael Lawless is a globally recognized professional with years of experience in laser eye surgery. He was the president of International Society of Refractive surgery in 2001 and a Chairman of the Department of Ophthalmology at Royal North Shore Hospital and Northern Area Health Service 2000 – 2006. As the first Australian surgeon to perform a laser cataract surgery, Professor Lawless is truly among the distinguished Australian experts in the field.
About Professor Alpins
Noel Alpins, MD, FACS, has been practicing cataract surgery and refractive surgery for over three decades, which has brought him international recognition and a status of a leading authority in the field. He was also awarded the 2012 International Society of Refractive Surgery (ISRS) and American Academy of Ophthalmology (AAO) Lans Distinguished Award in Chicago.